Last Monday, 4/10, I went in to my oncologist, Dr. Hu, to schedule the follow-up chemo we had agreed to a long time ago, before the surgeries. I had been keeping them updated through emails, mainly to ask for yet another refill of the Fentanyl patch because my reconstruction had been delayed, yet again.
I was expecting a very simple consultation where we set our start date and discussed the new agent we were going to be using. They had mentioned Doxil, or doxorubicin, in passing, in an email, so Mark had done some of his own research on it. It is a liposomal version of adriamycin, one of the dreadful chemos I had fared so poorly with before, but because in this form the molecules of chemo are encapsulated in fat, the delivery mechanism was changed. It minimizes the heart damage and nausea. I might not even lose my hair this time. But mouth sores and peripheral neuropathy are still a distinct possibility.
Okay. That doesn’t sound so bad.
But what my oncologist said when I finally saw him was not, “Okay, let’s get started.” It was “There’s a complication. We’re going to get another CT scan, and then decide how to proceed.?”
“What? Why? Has something changed?”
“Well, protocol usually dictates that we initiate the follow up chemo within 84 days of the tumor removal.”
And then my head started spinning and my stomach clenched. My tumor was removed at the beginning of December. It is now the beginning of April. The repeated delays in the manufacture of the prosthesis had pushed out my reconstruction incrementally, weeks at a time, to three full months after the tumor extraction. Then there was the requisite month of healing before chemo. Did I miss some kind of deadline I wasn’t even aware of? Was there no point in the follow up chemo because it was too late? Any micrometastases I might have had were beyond treating? AM I DYING NOW BECAUSE WE’RE PAST 84 DAYS?
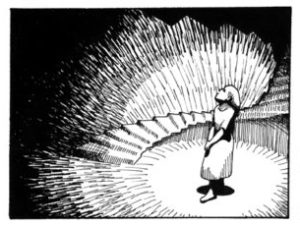
Which reminded me of an observation I made to Mark the night before, that I thought anyone who ever had cancer had forever stuck in the back of their heads an addendum to any response made to the common question “How are you?” That no matter how far out of the process you are, the specter of recurrence is always with you. You respond normally,
“Oh fine.” But in your head you continue with,
“So far.”
“For now.”
“Until the next scan comes back positive.”
But we don’t say that part out loud because, while truthful, it’s a downer at parties. And really, any of us could get hit by a bus tomorrow.
But what I very calmly said to my oncologist was, “What’s so magical about the number 84? It sounds a bit arbitrary.”
He shrugged and said, “That’s just clinically how we do it.”
“So, we’ll get the scan and see if anything shows up? How long does it take for a metastasis to become detectable anyway?”
“They’re detectable at about a centimeter, and it takes the average tumor about six months to get that big from a micrometastasis.”
“Well it hasn’t been six months yet… Ah. Mine wasn’t an AVERAGE tumor. So it might show up this early. So. So… If nothing shows up on the CT scan, we assume that IF I have micrometastases, then they are still as susceptible, IF they were even susceptible in the first place, to chemo as they would have been within 84 days, and we proceed as planned.” (So many caveats.) “If something shows up on the scan, then what? How do we do things different?”
“Well. If that’s the case, then we have to come up with a new plan. Probably a new combination of surgery and chemo… Let’s leave that discussion for if it comes up (i.e. I should make sure my will is in order). We’ll schedule you for the CT scan and bloodwork this Wednesday. If that looks good we’ll start the chemo as planned next Monday. We’ll go ahead and make that appointment too.”
“So I won’t find out what we’re doing Monday until I get here.”
“No. No. Email us when you’re done with the scan and we’ll take a look at it and get back to you right away.”
A tense couple of days later, during which Mark and I very pointedly didn’t discuss the potential results, and Kristi, the member of the oncology team who had kindly been renewing my Fentanyl patches, emailed me the same night to tell me my scan was clear. THE SCAN WAS CLEAR. I AM NOT DYING (yet).
They were really busy on Monday, 4/17, when I went in for the chemo. I ended up at the cancer center 8 hours for a 3 hour transfusion. It gave me some time to chat with some of the people there.
The cheerful, well-dressed and coiffed, chatty grandma across the way knew all the nurses because her colon cancer, gone for 5 years, had come back and was now everywhere, including, coincidentally, a bone in her shoulder. We bonded over how yes, actually, that is quite painful. When she left she gave me a concerned look, meant to be reassuring maybe, and stuttered, “But I hope you don’t have any, I mean I wish you all the best.. You probably won’t have any.. Well. I hope everything goes well.” She was too self-consciously aware of providing the object proof to the fear we all walk around with. She wanted me to know that just because it happened to her, didn’t mean it would happen to me, and even if it did, she had managed her metastases on and off chemo and with surgeries for another six years after the recurrence. And still managed to be dapper.
I got the message.
Later one of the nurses brought me some literature on the drug, since I hadn’t had it before. I’m glad she did, because while I knew about the potential peripheral neuropathy, apparently it’s a little bit different with this drug. The liposomal delivery system gives it a propensity to collect in the hands and feet, and can cause open sores, especially if you expose your extremities to too much friction or heat, like cooking, or too-hot baths (nooooooo not the hot bath).
And just as we were discussing this, the disembodied voice of the man in the next chair over, on the other side of the privacy curtain, volunteered, “Oh yeah. That happened to me. About two months after the chemo, I lost so much skin on my hands that I couldn’t so much as lift a water glass for two weeks.”
So my infusion was yesterday. I didn’t sleep last night. I thought I would crash today, but don’t really feel tired yet. I don’t know if it’s a side effect of all the changing levels of too many chemicals in my body, or if it’s more psychological. I’m waiting to start vomiting my lungs out. Or for my hands to flat out rot off of my wrists.
But so far, the first day after my only infusion for the next three weeks, I feel completely … normal.
I keep waiting for the hammer to fall.
But maybe.
Maybe it will be fine.
Leave a Reply